When Nestor Montalvo awoke one morning last September in his Long Island home, he was met with a disorienting headache and blurred vision. The symptoms felt akin to a “really bad hangover,” despite not having consumed any alcohol the previous day. Attempting to stand, Montalvo discovered the right side of his body was numb, leading to a frightening fall.
“Everything started spinning. I went to stand up, and I fell,” Montalvo, 61, recounted. “I just didn’t understand what was going on. I couldn’t understand it. I didn’t know why I was feeling that way.” His wife, alarmed by his condition, promptly called 911. Paramedics provided a chilling diagnosis: Montalvo was experiencing a stroke. He was rushed to the emergency room at Catholic Health’s Mercy Hospital in Nassau, Long Island, where the prognosis was grim. Overhearing a doctor inform his daughter, a registered nurse, Montalvo learned he had only a 15% chance of survival.
Understanding the Urgency: “Time is Brain”
Strokes occur when blood flow to the brain is obstructed by a blocked or ruptured blood vessel, explained Dr. Taylor Kimberly, chief of neurocritical care at Massachusetts General Hospital. Although not involved in Montalvo’s care, Kimberly emphasized the critical nature of timely treatment, encapsulated in the medical adage, “Time is brain.”
Montalvo suffered an ischemic stroke, a type where a blockage prevents brain cells from receiving essential nutrients and oxygen. The longer such a stroke remains untreated, the greater the potential for irreversible damage. Dr. Cini Thayil, the emergency medicine attending at Mercy Hospital, noted Montalvo’s “very prominent” neurological deficits upon his arrival, triggering the hospital’s stroke protocol.
“You could see that something was awry,” Thayil remarked.
Within minutes, Montalvo was assessed as a potential stroke patient and underwent a CAT scan. He was administered a clot-busting medication, TNK, and later underwent a minor procedure to ensure the clot’s removal. “I could have been a vegetable, I could have died,” Montalvo stated, acknowledging the life-saving interventions he received.
A Complicated Road to Recovery
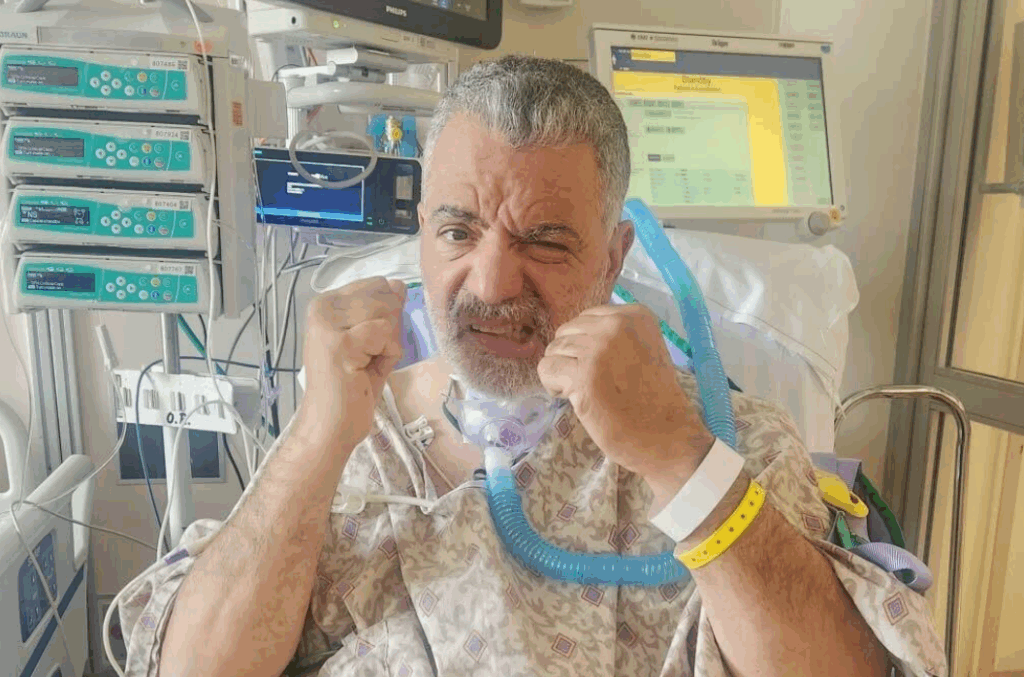
Despite the swift medical response, Montalvo’s challenges were far from over. The stroke had caused his vocal cords to collapse, necessitating a tracheotomy to assist his breathing. He was unable to speak or swallow due to the tubes and the stroke’s aftereffects, making basic functions like eating and talking arduous.
Aileen Fairchild, an acute care speech pathologist at Mercy Hospital, began working with Montalvo, who initially struggled to swallow even a quarter-teaspoon of applesauce. “It was a mess. I couldn’t swallow, I couldn’t talk, I couldn’t eat,” Montalvo recalled.
Over six weeks, Fairchild provided daily speech therapy and exercises targeting the throat muscles essential for swallowing. Regular scans monitored his progress. Following the removal of the tracheotomy tube, Montalvo underwent three additional procedures to further aid his recovery. By Thanksgiving, he was able to enjoy a regular meal with his family.
The Long-Term Impact and Future Outlook
Now, a year after his stroke, Montalvo has made significant strides. He can speak and eat as he did before, relishing retirement with his family and their dog, Paris. Though he still relies on a cane for mobility and continues outpatient physical therapy, Montalvo remains optimistic about his ongoing recovery.
“You take life for granted, and then when something like this happens, it wakes you up,” Montalvo reflected. “You hear people talk about it, and it just sounds like it’s not going to happen to you. All of a sudden, it happens to you.”
Montalvo’s experience underscores the importance of recognizing stroke symptoms and seeking immediate medical attention. His journey from a dire diagnosis to a hopeful recovery serves as a powerful reminder of the resilience of the human spirit and the critical role of timely medical intervention.