Health
B.C. Health Minister Proposes Cuts to Virtual Group Treatment

Concerns are rising among patients and healthcare providers in British Columbia as the provincial government plans to implement a cap on virtual group treatment sessions for chronic illness. The proposed changes, which are part of budgetary measures to address an anticipated deficit, could significantly impact access to critical health services for many vulnerable individuals.
The B.C. Centre for Long Covid, ME/CFS and Fibromyalgia employs a hybrid model that combines one-on-one appointments with virtual group sessions. According to co-founder Dr. Ric Arsenau, the centre has seen a remarkable success rate: 88 percent of patients report improvement in their conditions, while 17 percent have returned to work. Currently, each group session accommodates 50 patients, allowing individuals from across the province to connect and receive support.
Dr. Arsenau has expressed concern over the government’s plan to limit group sizes to 20 participants, arguing that this would render the virtual sessions unfeasible and potentially diminish the quality of care. He emphasized the program’s value, stating, “We save $1.2 million a year to the health-care system and we free up time for family doctors, emergency doctors and specialists.” This claim is supported by a social impact study conducted by MNA.
The demand for services at the B.C. Centre is growing, with approximately 6,000 British Columbians currently receiving care, a number that increases by about 2,000 each year. Patients who have endured years of misdiagnosis have found hope and validation at the clinic.
Denise Atkin, a patient who has battled chronic fatigue syndrome, described her experience as transformative. After becoming severely incapacitated by COVID-19, she found essential support through the virtual sessions. “This is my only access to safe, effective and informed medical care,” Atkin stated, noting her anxiety over the proposed changes.
Another patient, Dasha Axxelson, a former nurse, echoed similar sentiments. She emphasized the advantages of the format, which allows ample time with specialists who understand complex chronic conditions. “These are all people who actually specialize in complex chronic conditions,” Axxelson remarked, expressing gratitude for the accessibility that virtual care provides.
The Ministry of Health had initially expanded the Medical Service Plan (MSP) to include virtual care during the COVID-19 pandemic. However, the current review of this policy comes after reports that some physicians billed the MSP nearly $3,000 for one-hour sessions involving 100 patients. Health Minister Josie Osborne acknowledged the need for oversight, stating, “It is important that we put some parameters around this program for physicians so that it’s being delivered in a way that’s fiscally responsible.”
Despite these changes, Osborne assured the public that the government does not intend to eliminate remote access to health care. “We’re not limiting the ability for it to be provided virtually,” she clarified, indicating that stakeholder feedback would be taken into consideration before the proposed cap is finalized. The implementation is scheduled for early January 2024.
As discussions continue, both patients and healthcare providers remain hopeful that their voices will be heard in shaping the future of virtual health services in British Columbia.
-

 Politics1 month ago
Politics1 month agoSecwepemc First Nation Seeks Aboriginal Title Over Kamloops Area
-

 World5 months ago
World5 months agoScientists Unearth Ancient Antarctic Ice to Unlock Climate Secrets
-

 Entertainment5 months ago
Entertainment5 months agoTrump and McCormick to Announce $70 Billion Energy Investments
-

 Lifestyle5 months ago
Lifestyle5 months agoTransLink Launches Food Truck Program to Boost Revenue in Vancouver
-

 Science5 months ago
Science5 months agoFour Astronauts Return to Earth After International Space Station Mission
-

 Lifestyle3 months ago
Lifestyle3 months agoManitoba’s Burger Champion Shines Again Amid Dining Innovations
-
 Technology3 months ago
Technology3 months agoApple Notes Enhances Functionality with Markdown Support in macOS 26
-

 Top Stories2 months ago
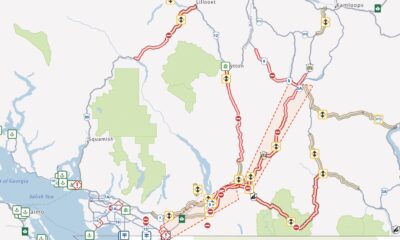
Top Stories2 months agoUrgent Update: Fatal Crash on Highway 99 Claims Life of Pitt Meadows Man
-

 Top Stories2 weeks ago
Top Stories2 weeks agoHomemade Houseboat ‘Neverlanding’ Captivates Lake Huron Voyagers
-

 Politics4 months ago
Politics4 months agoUkrainian Tennis Star Elina Svitolina Faces Death Threats Online
-

 Sports5 months ago
Sports5 months agoSearch Underway for Missing Hunter Amid Hokkaido Bear Emergency
-

 Politics5 months ago
Politics5 months agoCarney Engages First Nations Leaders at Development Law Summit