Health
Canadians Struggle with Insomnia Treatment, Experts Warn

Insomnia disorder affects more than 16 percent of Canadians, yet many are not receiving appropriate treatment, according to sleep expert Rébecca Robillard. As the director of clinical sleep research at the University of Ottawa Institute of Mental Health Research and co-chair of the Canadian Sleep Research Consortium, Robillard emphasizes the disconnect between awareness of sleep issues and the availability of effective treatment options.
Chronic insomnia, characterized by persistent difficulty in falling or staying asleep at least three times a week for a minimum of three months, poses serious health risks. Robillard notes that it can adversely affect individuals’ overall health, safety, cognitive abilities, and relationships. Despite a growing societal focus on achieving quality sleep, many Canadians remain without access to evidence-based therapies.
Current Treatment Approaches Fall Short
In light of this situation, Ontario Health has released new quality standards aimed at improving care for insomnia disorder. These standards advise that cognitive behavioral therapy (CBT) be prioritized as the first-line treatment. CBT focuses on modifying thoughts and behaviors that disrupt sleep and is widely regarded as the most effective long-term solution for insomnia.
Despite these recommendations, Robillard reports that approximately 98 percent of primary care providers in Canada still advocate for basic sleep hygiene practices as an initial response. These practices include maintaining a consistent sleep schedule, limiting screen time, and avoiding large meals or stimulants before bedtime. However, evidence supporting these methods is lacking, and they may inadvertently worsen the condition by fostering self-blame among patients.
“Sleep hygiene doesn’t work,” Robillard asserts. She warns that emphasizing these practices can reinforce the harmful belief that individuals simply need to try harder to sleep better, perpetuating cycles of anxiety and ineffective coping strategies.
Access to Effective Treatments Remains Limited
The recent quality standards from Ontario Health include several essential recommendations. They stress the need for comprehensive assessments for suspected insomnia disorder, the creation of tailored care plans, timely access to treatment for both insomnia and related health issues, and ensuring that patients can access CBT promptly. Furthermore, if medications are deemed necessary, they should be prescribed at the lowest effective dose for the shortest duration.
A significant barrier to effective treatment is access. Many Canadians lack primary care, and studies indicate that a substantial number of primary care physicians feel unprepared to manage insomnia disorder effectively. As a result, they often resort to promoting sleep hygiene instead of referring patients to appropriate therapies.
Robillard points out that while encouraging “healthy sleepers” to adopt good habits is beneficial, presenting sleep hygiene as a solution for clinical insomnia can be detrimental. It reinforces the notion that individuals are not trying hard enough, which is particularly concerning for those already struggling with sleep issues.
Surveys reveal that around 43 percent of respondents reported a previous diagnosis of insomnia disorder. However, many individuals do not seek professional assessment and may resort to self-medication with over-the-counter drugs or alcohol, further complicating their conditions.
One of the challenges with CBT is the limited availability of trained therapists. To address this issue, the Canadian Sleep Research Consortium is developing digital self-help tools designed to improve accessibility for patients facing insomnia. These resources aim to provide support and guidance for those seeking effective treatment.
As the conversation around sleep continues to grow, it is crucial for patients and healthcare providers to engage with current evidence-based practices. Addressing the treatment gap for chronic insomnia can lead to improved health outcomes and overall well-being for many Canadians.
-

 Politics2 weeks ago
Politics2 weeks agoSecwepemc First Nation Seeks Aboriginal Title Over Kamloops Area
-

 World4 months ago
World4 months agoScientists Unearth Ancient Antarctic Ice to Unlock Climate Secrets
-

 Entertainment4 months ago
Entertainment4 months agoTrump and McCormick to Announce $70 Billion Energy Investments
-

 Lifestyle4 months ago
Lifestyle4 months agoTransLink Launches Food Truck Program to Boost Revenue in Vancouver
-

 Science4 months ago
Science4 months agoFour Astronauts Return to Earth After International Space Station Mission
-
 Technology3 months ago
Technology3 months agoApple Notes Enhances Functionality with Markdown Support in macOS 26
-

 Top Stories1 month ago
Top Stories1 month agoUrgent Update: Fatal Crash on Highway 99 Claims Life of Pitt Meadows Man
-

 Sports4 months ago
Sports4 months agoSearch Underway for Missing Hunter Amid Hokkaido Bear Emergency
-

 Politics3 months ago
Politics3 months agoUkrainian Tennis Star Elina Svitolina Faces Death Threats Online
-

 Politics4 months ago
Politics4 months agoCarney Engages First Nations Leaders at Development Law Summit
-

 Technology4 months ago
Technology4 months agoFrosthaven Launches Early Access on July 31, 2025
-
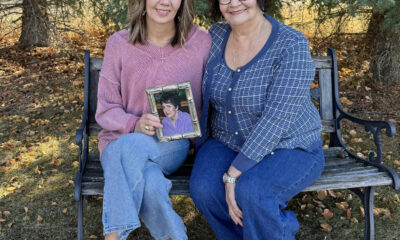
 Top Stories3 weeks ago
Top Stories3 weeks agoFamily Remembers Beverley Rowbotham 25 Years After Murder









