Health
Chinese Man Survives 171 Days With Genetically Modified Pig Liver
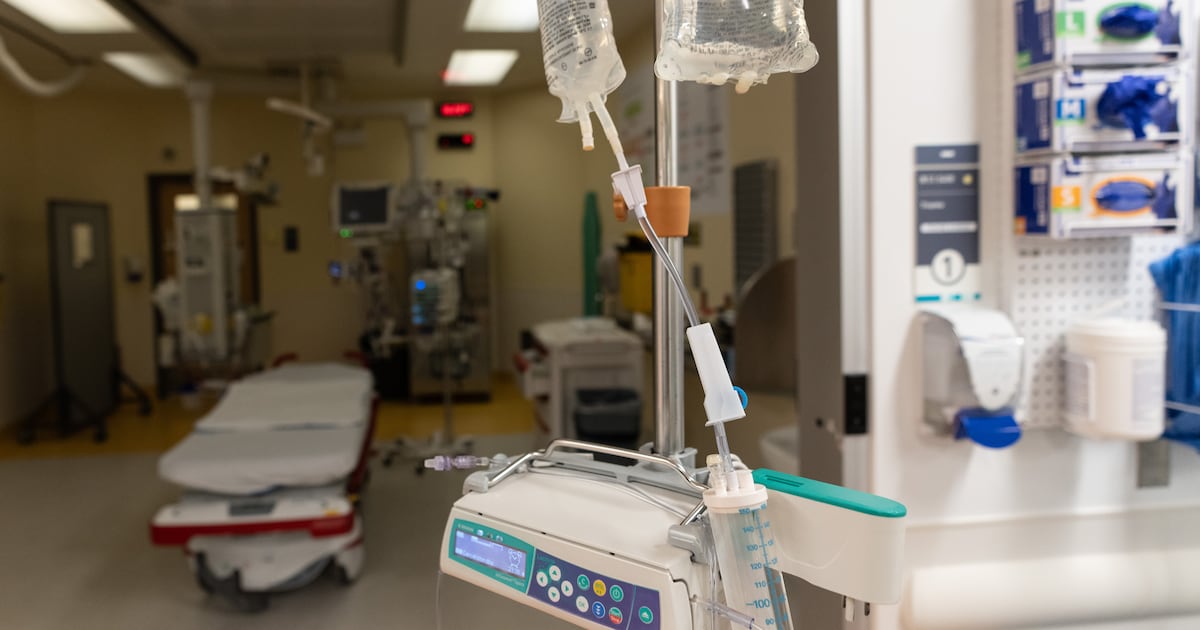
A 71-year-old man in China lived for 171 days after receiving a genetically modified pig liver transplant, marking a significant milestone in the field of xenotransplantation. The procedure, conducted in May 2024 at the First Affiliated Hospital of Anhui Medical University, involved a liver from a genetically altered pig designed to minimize the risk of organ rejection.
This pioneering case represents a step forward in the use of animal organs for human transplantation. While previous successes have included pig kidneys and hearts, the liver’s complexity posed challenges to its viability as a transplant candidate. Dr. Beicheng Sun, the hospital’s president and co-author of the study published in the Journal of Hepatology, expressed optimism about the future of liver transplants from pigs, stating, “I think liver is good if we can get enough human genes in the pig.”
The liver performs multiple critical functions, including filtering blood, detoxifying harmful substances, and producing proteins essential for blood clotting. Given its size and dual blood supply, replacing it with a pig organ is significantly more complicated than with other organs such as kidneys or hearts.
Last year, Penn Medicine achieved the world’s first successful external liver perfusion using a gene-edited pig organ, demonstrating the organ’s potential for human application. The findings from this latest study suggest that pig livers could serve as a bridge for patients with severe liver conditions, allowing time for recovery or for a human donor liver to become available.
In the case discussed in the study, the patient suffered from hepatitis B-related cirrhosis and had a large tumor in his liver. After standard treatments failed, the transplant became the only viable option. Doctors discussed the experimental nature of the procedure with the patient and his family, who ultimately consented.
The surgical team transplanted the genetically modified liver onto the remaining healthy tissue of the man’s liver. Initial results were promising, with the pig liver exhibiting normal function within days. There were no signs of acute rejection in the first ten days post-surgery, and the left side of the patient’s liver appeared to be functioning better than before.
Despite early success, challenges arose as the patient began to show signs of stress related to the transplant. By day 38, doctors determined that the man’s native liver could sustain his body without the pig organ, leading to the removal of the transplant. The patient continued to function well for some time following the removal, although he later developed gastrointestinal bleeding and passed away 171 days after the initial procedure.
The research highlights the potential for pig-to-human liver transplantation to provide temporary support for patients facing liver failure. According to the study authors, this approach could enable patients to survive long enough for their own liver to recover or for a human organ to become available.
Dr. Heiner Wedemeyer, a professor at Hannover Medical School, noted the study’s significance, describing it as a cause for cautious optimism for the future of organ transplantation. He emphasized the groundbreaking nature of the findings, suggesting that they could provide new opportunities for patients in critical need of liver support.
As the demand for organ transplants continues to grow, with over 100,000 individuals on waiting lists in the United States alone, innovative solutions like xenotransplantation are becoming increasingly important. With more than 9,000 people waiting for a liver transplant, the exploration of pig organs as a viable alternative may hold the key to addressing the ongoing organ shortage crisis.
-

 Politics4 weeks ago
Politics4 weeks agoSecwepemc First Nation Seeks Aboriginal Title Over Kamloops Area
-

 World5 months ago
World5 months agoScientists Unearth Ancient Antarctic Ice to Unlock Climate Secrets
-

 Entertainment5 months ago
Entertainment5 months agoTrump and McCormick to Announce $70 Billion Energy Investments
-

 Science5 months ago
Science5 months agoFour Astronauts Return to Earth After International Space Station Mission
-

 Lifestyle5 months ago
Lifestyle5 months agoTransLink Launches Food Truck Program to Boost Revenue in Vancouver
-
 Technology3 months ago
Technology3 months agoApple Notes Enhances Functionality with Markdown Support in macOS 26
-

 Lifestyle3 months ago
Lifestyle3 months agoManitoba’s Burger Champion Shines Again Amid Dining Innovations
-

 Top Stories2 months ago
Top Stories2 months agoUrgent Update: Fatal Crash on Highway 99 Claims Life of Pitt Meadows Man
-

 Politics4 months ago
Politics4 months agoUkrainian Tennis Star Elina Svitolina Faces Death Threats Online
-

 Sports5 months ago
Sports5 months agoSearch Underway for Missing Hunter Amid Hokkaido Bear Emergency
-

 Politics5 months ago
Politics5 months agoCarney Engages First Nations Leaders at Development Law Summit
-

 Technology5 months ago
Technology5 months agoFrosthaven Launches Early Access on July 31, 2025




















