Top Stories
UBC Breakthrough Converts Kidney for Transplant, Major Progress!

BREAKING: A revolutionary kidney transplant using an enzyme technology from the University of British Columbia (UBC) has just been confirmed as a success, marking a pivotal advancement toward universal donor organs. This breakthrough, published today in Nature Biomedical Engineering, signals a potential game-changer for thousands of patients awaiting kidney transplants.
In a groundbreaking first-in-human trial, researchers successfully converted a kidney from type A blood to the universal type O, preventing organ rejection. The transplant occurred in late 2023 into a brain-dead recipient, with family consent, allowing researchers to monitor the immune response without endangering a life. For an impressive two days, the kidney functioned seamlessly, free from signs of hyperacute rejection, a dangerous immune reaction that can destroy incompatible organs within minutes.
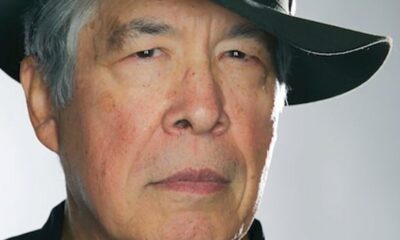
Dr. Stephen Withers, professor emeritus of chemistry at UBC and a co-leader of the enzyme development, stated, “This is the first time we’ve seen this play out in a human model. It gives us invaluable insight into how to improve long-term outcomes.” By the third day, minor blood-type markers reappeared, resulting in a mild immune reaction, but the response was significantly less severe than typical mismatches, indicating that the body was beginning to accept the organ.
This monumental achievement is the culmination of over a decade of research. In the early 2010s, Dr. Withers and colleague Dr. Jayachandran Kizhakkedathu focused on creating universal donor blood by removing sugars that define blood types. The same sugars coat organ blood vessels, triggering immune responses against mismatched transplants. With over half of kidney waitlist patients being type O, this innovation could drastically reduce their waiting time, which often spans two to four years, leading to preventable deaths.
Conventional methods to address blood-type incompatibility in transplants are lengthy and complex, requiring intensive treatments to suppress the immune system and typically relying on living donors. UBC’s new approach alters the organ instead of the patient, expediting transplant procedures with fewer complications and unlocking the potential for utilizing organs from deceased donors—where every moment is critical.
The key to this remarkable innovation lies in the discovery of two highly effective enzymes by the UBC team in 2019. These enzymes efficiently remove the sugar that characterizes type A blood, effectively converting it to type O. Dr. Kizhakkedathu remarked, “These enzymes are highly active, highly selective, and work at very low concentrations. That made the whole concept feasible.”
After successful tests on blood and lungs, the decisive question remained: could an enzyme-converted organ survive within a human immune system? The answer emerged during a 2023 overseas trip, when collaborators revealed successful data confirming the kidney’s performance in a brain-dead recipient. “I was so thrilled. It was a dream moment,” Dr. Kizhakkedathu recalled.
The enzymes function like molecular scissors, removing the ‘nametag’ that identifies type A blood, thus rendering the organ unrecognizable to the immune system. Dr. Withers illustrated this breakthrough by comparing it to removing red paint from a car to reveal a neutral primer underneath. “Once that’s done, the immune system no longer sees the organ as foreign,” he explained.
Looking ahead, regulatory approval for clinical trials is the next challenge. The UBC spin-off company Avivo Biomedical will spearhead the development of these enzymes for transplant applications and facilitate the creation of universal donor blood on demand for transfusion needs.
“This is what it looks like when years of basic science finally connect to patient care,” Dr. Withers stated. As researchers continue to push the boundaries of science, this breakthrough brings hope for a future where organ transplantation can save countless lives, making it imperative for the medical community and patients alike to monitor these developments closely.
-

 Politics4 weeks ago
Politics4 weeks agoSecwepemc First Nation Seeks Aboriginal Title Over Kamloops Area
-

 World5 months ago
World5 months agoScientists Unearth Ancient Antarctic Ice to Unlock Climate Secrets
-

 Entertainment5 months ago
Entertainment5 months agoTrump and McCormick to Announce $70 Billion Energy Investments
-

 Science5 months ago
Science5 months agoFour Astronauts Return to Earth After International Space Station Mission
-

 Lifestyle5 months ago
Lifestyle5 months agoTransLink Launches Food Truck Program to Boost Revenue in Vancouver
-
 Technology3 months ago
Technology3 months agoApple Notes Enhances Functionality with Markdown Support in macOS 26
-

 Lifestyle3 months ago
Lifestyle3 months agoManitoba’s Burger Champion Shines Again Amid Dining Innovations
-

 Top Stories2 months ago
Top Stories2 months agoUrgent Update: Fatal Crash on Highway 99 Claims Life of Pitt Meadows Man
-

 Politics4 months ago
Politics4 months agoUkrainian Tennis Star Elina Svitolina Faces Death Threats Online
-

 Sports5 months ago
Sports5 months agoSearch Underway for Missing Hunter Amid Hokkaido Bear Emergency
-

 Politics5 months ago
Politics5 months agoCarney Engages First Nations Leaders at Development Law Summit
-

 Technology5 months ago
Technology5 months agoFrosthaven Launches Early Access on July 31, 2025